SCIENCE EPISODE
Can You Reverse PCOS? The Science of Insulin & Hormones
I just want to stress how important it is if you have PCOS, if you know somebody who has PCOS, to understand insulin and how these PCOS symptoms could simply be your body’s reaction to having high insulin levels, and by using my glucose hacks and Anti-Spike you can get those down very quickly.
Hello angels and welcome back to the Glucose Goddess Show. I’m Jessie Inchauspé. I’m a French biochemist obsessed with helping you understand how your body works, and today we’re going to talk about PCOS, polycystic ovary syndrome.
I cannot tell you how many people I meet who have this condition and how they don’t have the right information to be able to help themselves. Let’s get into it. Polycystic ovary syndrome is now affecting one in five females worldwide. Can you imagine that? One in five — that is such a high number, it’s completely mad.
So PCOS is sort of an umbrella term that covers lots of different symptoms that you might have in a body due to hormonal imbalances. Specifically, PCOS covers symptoms caused by having too much testosterone — a male sex hormone — in a female body. Some of these symptoms are balding on the head, hair growth on the face, acne, missed periods, irregular periods, and little cysts on your ovaries that are preventing ovulation. But despite the name, you don’t need to have the cysts on your ovaries to still be considered to have polycystic ovary syndrome.
So again: PCOS equals a group of symptoms. The very first, most important thing you must know if you have PCOS is that you have to get your fasting insulin level checked. This is very, very key. I’m going to explain why in a second. So, little recap on insulin: what is insulin? When we eat carbs — things like starches (bread, pasta, rice, potatoes, oats) or sugars (anything from fruit to candy or cake) — these are carbs. When we eat these carbs, they go into our digestive system and there they transform into glucose molecules. Carbs are just long chains of glucose molecules waiting to be cut and waiting to arrive into your bloodstream. After you eat carbs, glucose increases in your bloodstream. Your body, in response to this glucose increase (also called a blood sugar increase), does something really cool: it calls up your pancreas and goes, “Hey pancreas, can we please have some insulin in here?” because insulin is going to help take the excess glucose and store it away into your liver, into your muscles, and into your fat cells. This is very important because if glucose levels stay high for too long, that causes a lot of damage in our body.
The thing is, over time, as you spike your glucose levels over and over again and your body needs more and more insulin to put that extra glucose away, your body becomes what’s called insulin resistant. It’s the same thing as when I was a teenager and I started drinking coffee: the first time I had a cup of coffee I was like, “Whoa, this is so strong,” and then after about a year I needed three cups of coffee just to wake up in the morning. The same dose of coffee was no longer having that same strong effect — I had become resistant to caffeine, meaning I needed more and more of it to get the same effect. Well, your body over time becomes resistant to insulin — that’s what’s called insulin resistance.
Let me give you examples of some foods that will probably make your insulin levels go up and up over the years, and you might think these foods are actually really good and healthy.
Breakfast: fruit smoothie with some toast — glucose spike, insulin spike.
Lunch: sandwich with some low-fat cream cheese and a chocolate bar — carbs, glucose spike, insulin spike.
Snack: an oat-milk coffee or a fruit juice — again glucose spike, insulin spike.
Dinner: some veggies and lots of carbs like bread, pasta, rice, potatoes, and then for dessert maybe some low-fat ice cream — again, mostly carbs; these are going to create glucose spikes and insulin spikes and, over the years, cause your insulin levels to increase as you become more and more insulin resistant.
If you’re not sure what foods are carbs and what foods are not carbs, in the description of this episode I have a free PDF for you — my Food Classification Master List — and it’ll show you very precisely, with a long list of foods, which are going to increase your glucose levels and which are not.
So if this feels a bit murky and you’re not sure, download it — it’s free, it’s going to help you see more clearly. Okay, so now you should know it’s extremely common to have high insulin levels. The standard reference range tells us that “normal” fasting insulin levels are 25 micro–units per milliliter (or, if you’re in a different country and your units are different, 150 picomoles per liter). If you’re below this threshold, most people, most doctors, most medical professionals will say, “You’re fine, don’t worry about it.” The problem is this is not the threshold to thrive; this is the threshold like when we say a fasting glucose level under 100 mg/dL is fine because you’re not prediabetic — in fact, we know that you should be closer to 85 mg/dL to really help your body thrive. For insulin it’s kind of the same thing. The objective that cutting-edge science is telling us is actually to try to stay below 10 micro–units per milliliter, and if you’re in picomoles, the goal should be less than 60 picomoles per liter or lower.
Now, if you’ve ever had your fasting insulin levels tested, go grab that number and compare it to this, but most people are much higher than this number. For example, there was a study done in 2023 that looked at the fasting insulin of over 5,000 people — “Fasting Indices of Glucose–Insulin Metabolism Across Lifespan and Prediction of Glycemic Deterioration in Children With Obesity From New Diagnostic Cutoffs.” This study showed that, on average, most of the population is above this cutoff of 10 micro–units per milliliter — most of us have a fasting insulin level much higher than this thriving cutoff. So again: go check your fasting insulin numbers and see where you stand. Now let’s circle back to PCOS — why am I talking about insulin so much? Because when, in the female body, there is too much insulin, this has a strong impact on your ovaries. Having high insulin in a female body tells your ovaries to produce more testosterone. Testosterone is the male sex hormone and, in a female body, when you have too much testosterone compared to the female sex hormones, this causes an imbalance which is the root cause of PCOS symptoms. In most cases you see high insulin levels being the cause of the high testosterone — of the ovaries producing more testosterone — and of PCOS. About 50% to 80% of females with PCOS do present with a lot of insulin in the body, but not always. There are some cases where the PCOS is not linked to having high insulin levels, which is why, if you have PCOS, it is so important that you go check your fasting insulin level so that you can see, “Oh, could my extra high insulin be causing my ovaries to produce this testosterone?” Because if that’s the case, you can reverse it, and I’m going to show you exactly how.
So get your fasting insulin levels checked, and don’t look so much at the reference range that comes with the test results because, again, that reference range does not represent where you really should be — it represents what “normal” is, but today these reference ranges are not really where you should be basing yourself.
You should be trying to get below the thresholds I just mentioned, and there’s a free PDF in the description of this episode where you can see all of these blood tests and my recommendations for the ranges. Download it, test your fasting insulin, then compare and see where you stand.
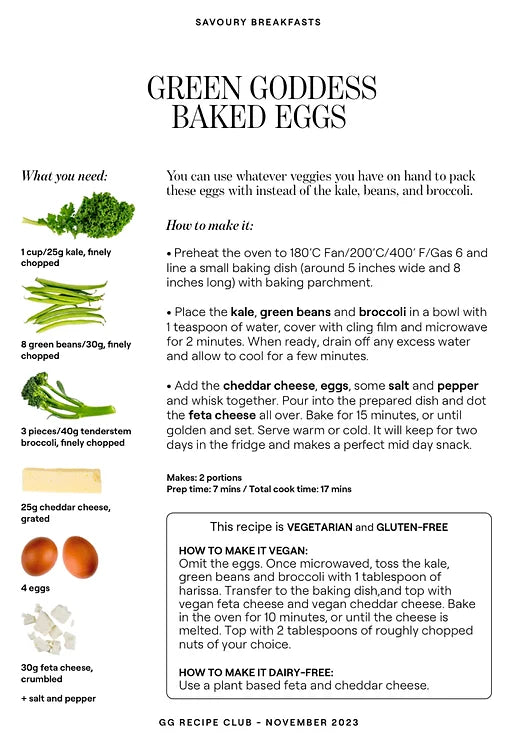
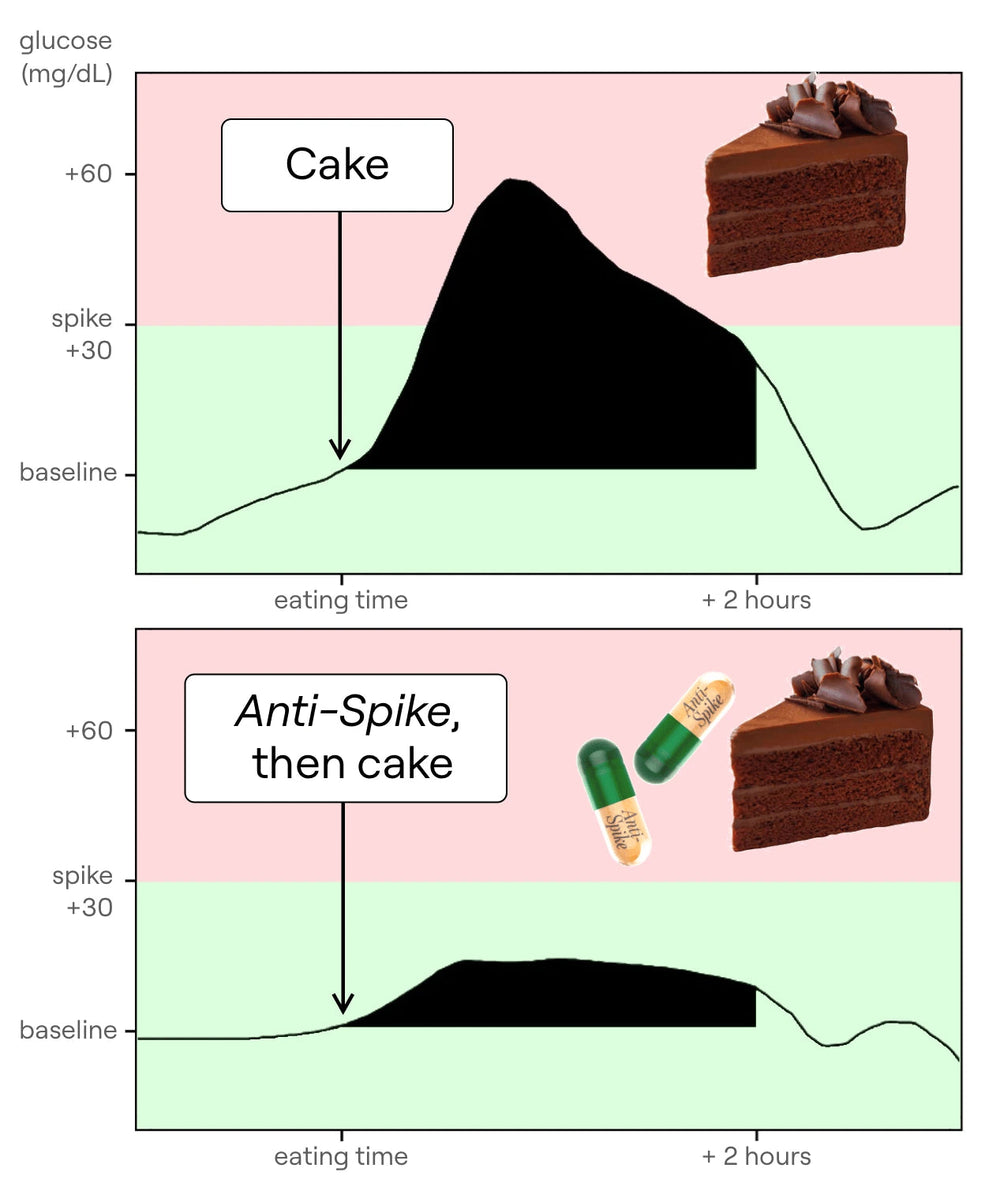
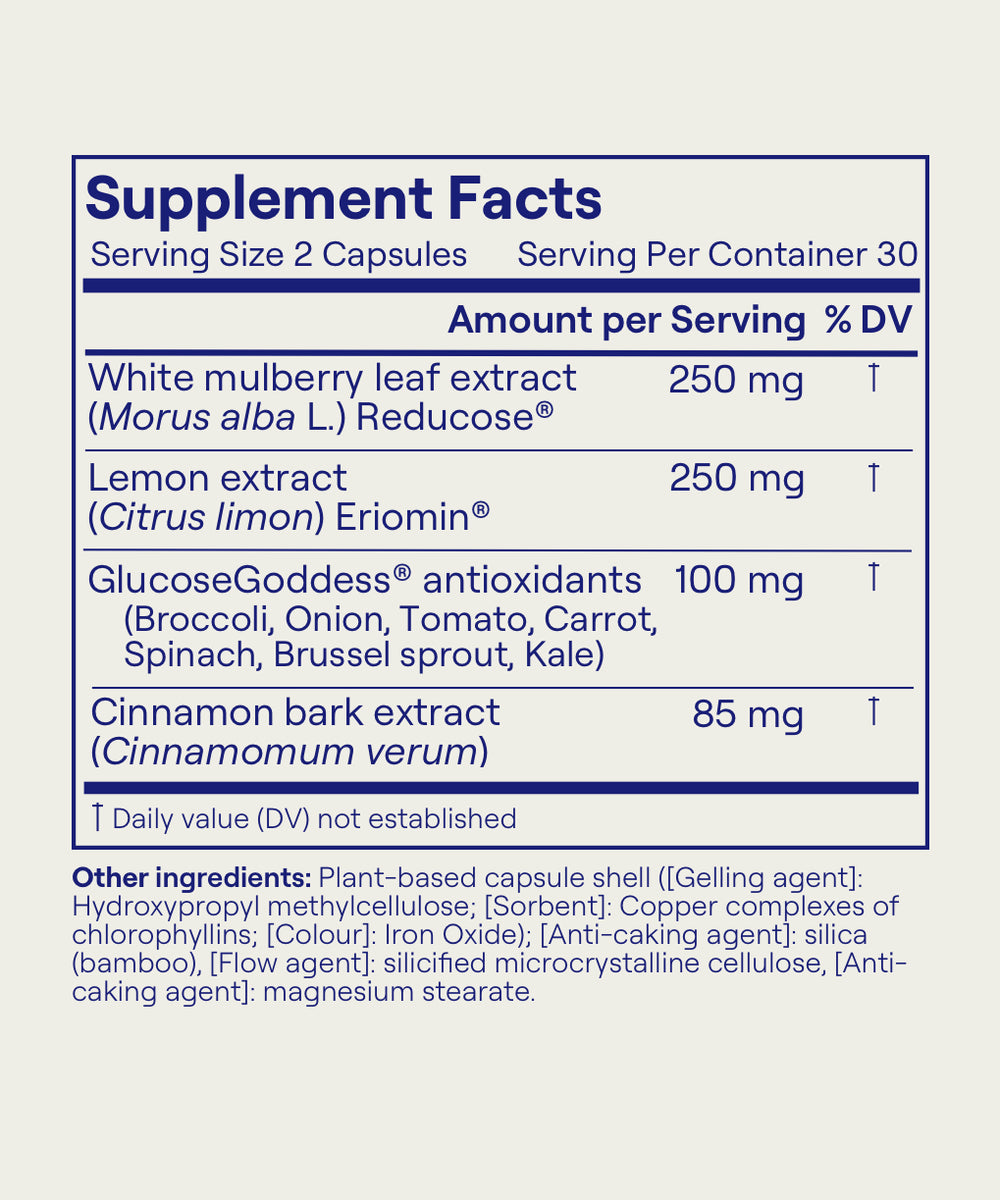
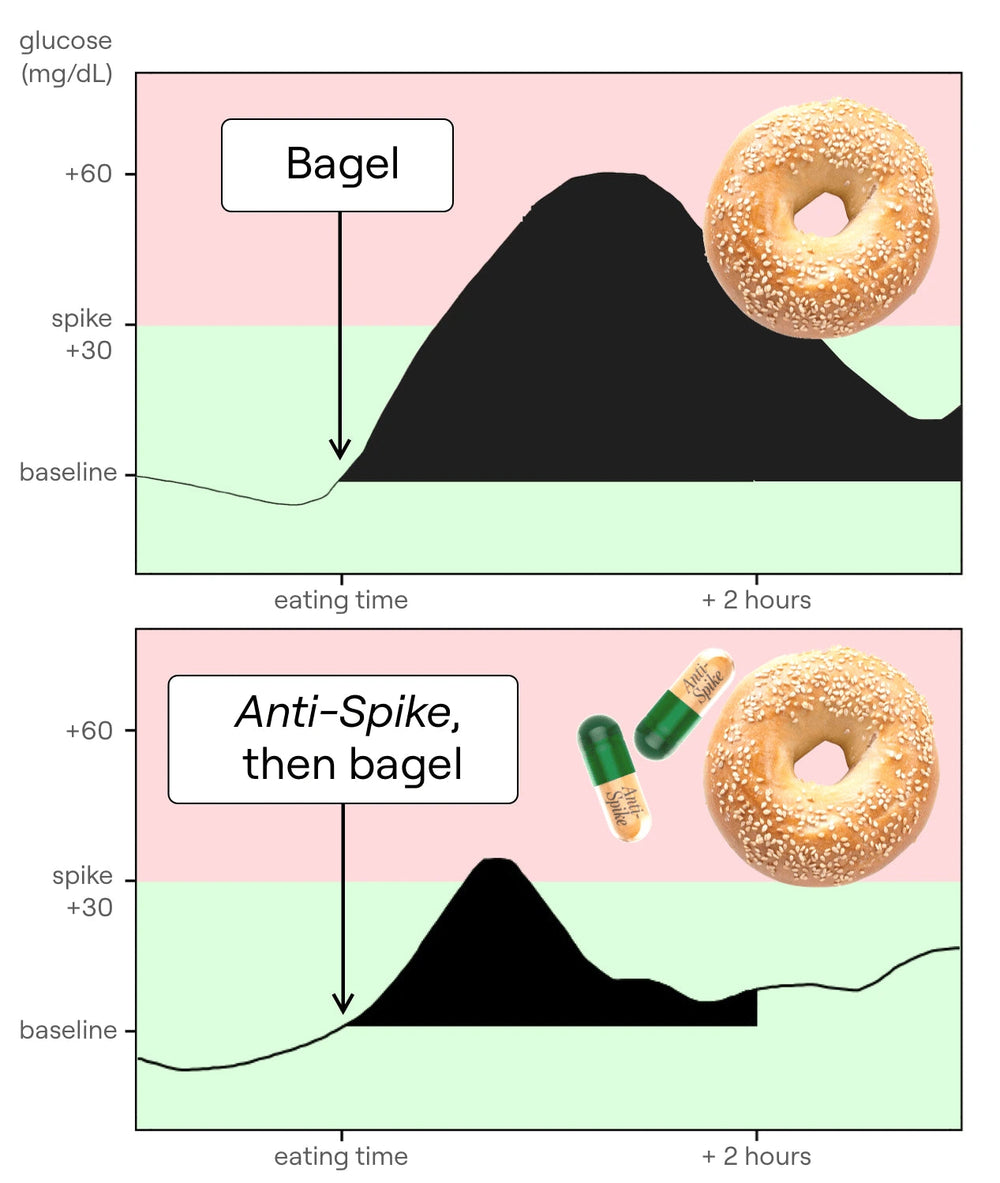
One important thing to note here is that having really high insulin is also the cause of type 2 diabetes — when you have a lot of insulin resistance over a very long time, that causes type 2 diabetes — and here are some really interesting statistics that show how much type 2 diabetes and PCOS are linked. The reason this is so important to understand is because type 2 diabetes, when you have it, you often don’t know; you can reverse it, but it is a reversible condition in most cases. PCOS is no different. Time for a quick break to tell you about the supplements I have developed — Anti-Spike Formula. Now listen, in my years of research I’ve understood one key thing: keeping our glucose levels steady is the foundation of physical and mental health, no question, and if you are currently battling PCOS this could be of great interest to you because science shows us that glucose levels and PCOS are tightly linked. I created Anti-Spike with two really powerful natural plant molecules in it. The first one is mulberry leaf extract — and listen to this: in a review study of 12 randomized clinical trials on over 600 people, scientists found that mulberry leaf extract significantly reduces our glucose spikes after a meal by up to 40%, it also significantly reduces our insulin spike after a meal by up to 40%, and it reduces our fasting glucose levels by 8 mg/dL after just two months. So this molecule from mulberry leaf reduces the absorption of glucose in our bloodstream — it actually slows down how quickly starches turn to glucose in our bloodstream — therefore creating a massive reduction in the glucose spike of our meal. The second main molecule in Anti-Spike Formula is a molecule from lemon called eriocitrine. It’s the molecule that makes lemons yellow, but it also has a really cool effect on our gut — it basically helps our guts produce more GLP-1. Clinical trials show us… I take Anti-Spike Formula every single day before the meal of my day highest in carbs and sugars. So go to anti-spike.com to see all the science behind these ingredients, to see testimonials from thousands of people who’ve tried it, and to order your own Anti-Spike Formula bottle and try it for yourself.
It’s not a condition that you are born with, it’s not something genetic that you can’t do anything about. If the root cause of it is these high insulin levels, well, reducing your insulin is going to help reduce all of your symptoms. So, again, studies that show the connection between PCOS and type 2 diabetes: the CDC says that over 50% of people with PCOS will develop type 2 diabetes by age 40, and this is much higher than the average — on average, about 10% of the population will develop type 2 diabetes, and a bit later than 40. Basically, if you have polycystic ovary syndrome and it’s caused by high insulin, you’re kind of on your way to getting type 2 diabetes because both of these conditions can often have the same root cause, which is high insulin levels. So, all this to say: well, if your PCOS is caused by high insulin levels, it should be really easy to fix it, right? You just do stuff to reduce your insulin levels. The problem is, today this is not something that is talked about at all, and generally if somebody has PCOS there’s going to be more of a treatment approach versus trying to regulate glucose and insulin levels first. If you have PCOS, you might be told to go on the birth control pill. Why? Because the birth control pill is just female hormones, and so as you have high testosterone in your body and then you take the birth control pill, the balance comes back to be about equal, so the symptoms go away because there’s female hormones to counterbalance the high testosterone. But the problem is, as soon as you stop taking the birth control pill, well, you have high testosterone again. I see this happen so often: people have been on the pill for a very long time for PCOS, then they want to have a baby, so they stop taking the pill, and then boom — all the symptoms come back because the testosterone is still really high and they’re not ovulating, they’re not getting their period, they cannot get pregnant. So the birth control pill is going to mask the symptoms — it’s not going to solve the root cause if the root cause is insulin resistance. That’s really, really important. You may actually also be given some diabetes medication to solve your PCOS because diabetes medication is going to reduce your glucose levels, but we can often do some things before we take medication that are not too complicated — my glucose hacks — that could significantly help you reduce your insulin resistance, reduce your insulin, reduce your testosterone, and get rid of your symptoms. I find this topic so important to discuss because I meet so many women who have PCOS and have no idea they can reverse it. So yeah, sorry, I’m a bit excited — slightly angry too — that this information is not more widely available, but hey, I’m doing my best.
Okay, so I’m going to go through a few of my hacks — my glucose hacks — that are going to help you reduce your glucose levels, reduce your insulin resistance. There’s another PDF in the description of this episode with all of my glucose hacks.
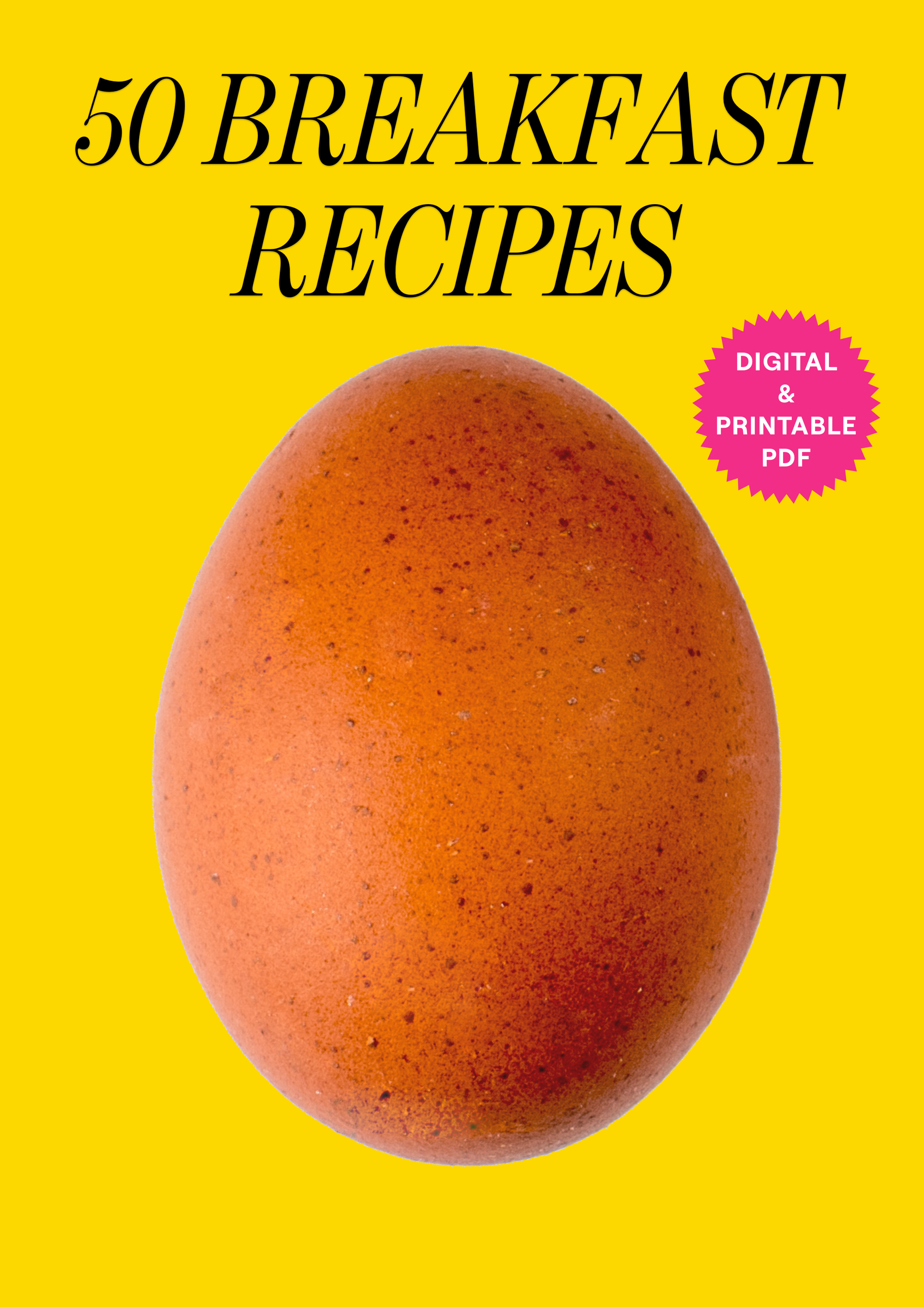
The first and most important thing is your breakfast, my dears: your breakfast should be savory, not sweet. Start your day with protein. For example, this morning I had my favorite two-egg omelet with feta and tomatoes. Start your day with something savory built around protein, because most of us create a massive glucose spike with our breakfast — juice and oats and some bread with jam — most of us create massive glucose and insulin spikes first thing in the morning. So: your breakfast should be savory.
Second: if you want to eat something sweet, which is fine, here’s how to do it with less of a glucose spike — make sure you’re eating the sweet food after a meal; never on an empty stomach, never as a snack, never first thing in the morning when your system is completely empty and very sensitive. Sugar is fine as long as it’s for dessert after a meal; never on its own.
Another really key hack here is “veggies first”: at the beginning of your lunch and your dinner, when it’s easy, add a plate of vegetables to the beginning of your meal, and then you can eat whatever you normally eat. By adding the plate of vegetables at the beginning of your meal, you’re going to create a protective mesh in your intestine; this protective mesh is going to prevent glucose molecules from arriving too quickly into your bloodstream when you eat carbs during the rest of your meal. That’s the veggie-starter hack.
Another good hack I want to share is vinegar: one tablespoon of vinegar once a day, diluted in water or added as a dressing on your veggie starter. This is going to reduce the glucose of your meals by up to 30%. There are even some studies linking vinegar and help with PCOS symptoms. Super-easy hack — have it before your biggest meal of the day.
Something else: I know that when we have PCOS — and this is what I hear from many of you — one of the main things you struggle with are cravings.
There are some really wonderful natural plant molecules that you can take to help with those. I recommend mulberry leaf before the biggest meal of your day — this is going to reduce the glucose spike of that meal very significantly, by up to 40%, with no effort. The second molecule I recommend you take is from lemon — it’s a lemon antioxidant that’s going to help reduce insulin resistance and reduce your fasting glucose levels over time, and also naturally increase the amount of GLP-1 produced by your gut cells. This will reduce cravings and reduce your constant hunger. So: mulberry leaf extract and lemon antioxidant — the best source of them is in my supplement called Anti-Spike (link in the description of this episode). So: my 10 hacks in the PDF, Anti-Spike once a day — the rest is history, seriously.
Let’s discuss weight loss now. I know this is a topic for many of you. You don’t need to lose weight to reduce your insulin levels; you don’t need to lose weight to help your body be healthier. But what happens generally is that when you get your glucose and your insulin levels under control, a few things fall into place: fewer cravings, less hunger, and with less insulin in your body, your body can burn more fat for fuel. This is good — this is not like a weight-loss thing about losing fat as quickly as possible. Burning fat for fuel is super important for your health; it’s called metabolic flexibility. When we reduce glucose and insulin levels, we’re able to be more metabolically flexible, to burn more fat for fuel, and fat is a wonderful source of energy for our body. As a consequence of using my hacks and Anti-Spike, usually people with PCOS will also lose fat on their body — again, as a consequence of everything becoming healthier, not as the main objective. Interestingly, some people with PCOS can present with very little body fat on their body.
There’s a 2021 study called “PCOS and Nutritional Approaches — Differences Between Lean and Obese Phenotype.” Essentially this study showed that no matter how much body fat you have, you can still have PCOS — which makes total sense because it’s not about having fat on your body; it’s about insulin levels — and that whatever your phenotype (meaning whatever your body size), improving your nutritional health — improving your diet using my hacks, reducing sugar intake, reducing processed carbs intake, going for more protein with my savory breakfast, more fiber with my veggie starter — these all help regardless of what your body looks like. You can have PCOS.
I want to mention two more studies because it’s really encouraging to see there’s more and more research being done on PCOS and our ability to reverse PCOS symptoms with our food. The first one: “Effects of a Ketogenic Diet in Women With Polycystic Ovary Syndrome.” This study shows that if you go for 12 weeks of no glucose spikes at all, you can improve all the key biomarkers of PCOS — testosterone levels, insulin, glucose. In this study it was quite extreme — they went on a keto diet (a diet with zero carbs whatsoever). This is challenging and can be very difficult to maintain, so I don’t recommend that, but it’s just to show you that in the scientific studies scientists are finding that, oh yeah, if we change how these females are eating, we see PCOS symptoms going away. With my glucose hacks, what’s quite cool is that you’re going to be able to get basically similar effects to that of a keto diet — reducing your glucose spikes, reducing your insulin levels — but in a less extreme way, in a way that allows you to still eat whatever you love. We’re not going to cut out carbs entirely — I don’t really believe in that; I think that’s not sustainable — but the key here is that this study shows that by reducing our glucose levels we can reduce our PCOS symptoms, and my glucose hacks are the easiest entryway to that new world of smaller glucose spikes. Another one on the topic of vinegar, which is so cool: “Intake of Vinegar Beverage Is Associated With Restoration of Ovulatory Function in Women With PCOS.” This study showed a daily tablespoon of vinegar for 40 days can help females with PCOS ovulate again — can help restore ovulatory function.
Vinegar is a very easy way to reduce your glucose spikes, and this study shows that just doing this for 40 days can help you ovulate again. So if you’re trying to ovulate — maybe you want to have a baby, maybe you just want regular periods because that’s such an important marker of female health — these hacks can really, really help you. And on the topic of vinegar: don’t just go and put vinegar on everything — it’s a cool hack, but you have to use it in combination with all of the other ones. Vinegar alone is not going to allow you to eat all the chocolate you want with no consequences; it’s just one of many hacks. So, my dears, we’re almost at the end of this episode. I just want to stress how important it is — if you have PCOS, if you know somebody who has PCOS — to understand insulin and how these PCOS symptoms could simply be your body’s reaction to having high insulin levels, and by using my glucose hacks and Anti-Spike you can get those down very quickly. I’m going to read you a few testimonials from people who’ve used my hacks with PCOS. Now of course, testimonials are not scientific studies — they’re just anecdotes — but I think they’re quite nice to hear.
First one: “I hadn’t ovulated in over five months due to PCOS, and by following the method (my glucose hacks) I was able to ovulate and get pregnant after two weeks. I was about to start ovulation medication, but thanks to doing this it happened naturally. My husband and I are over the moon.” Yeah — a lot of the conditions that we have, a lot of the symptoms that we feel every day, can be a consequence of having glucose and insulin levels that are out of whack. Food should be the first place we look for medicine, always. Another one: “By Anti-Spike — I have insulin-resistant PCOS and struggle a lot with sugar spikes and bloating. I sometimes get so uncomfortable halfway through a meal I can’t even finish it. I started taking Anti-Spike a few months ago, and it has made an immediate difference.”
So just to recap: get your fasting insulin levels checked, compare them to my blood-sugar PDF guide in the description of this episode, or even just start the hacks without doing the fasting insulin test — it doesn’t matter.
The hacks are going to be your best friends to try to fix PCOS through food first. So download my hacks, take Anti-Spike, and let me know how it goes. I see people reversing their PCOS in just a few weeks all the time in my readers of my books and in the online community we’ve created.
Please try it out, let me know how it goes — I can’t wait to hear your amazing results.
Lots of love, and I’ll see you next time.
 Anti-Spike Supplement
Anti-Spike Supplement
 The Recipe Club
The Recipe Club
 Course
Course
 50 Breakfast Recipes
50 Breakfast Recipes
 50 Veggie Starter Recipes
50 Veggie Starter Recipes
 20 Vegan Recipes
20 Vegan Recipes
 20 Gluten-Free Recipes
20 Gluten-Free Recipes
 The 10 Glucose Hacks
The 10 Glucose Hacks
 Vinegar
Vinegar
 Alcohol
Alcohol
 Fasting
Fasting
 GLP-1
GLP-1
 What to Eat Before & After Exercise
What to Eat Before & After Exercise
 Protein
Protein
 PCOS
PCOS
 Menopause
Menopause
 My MRI Story
My MRI Story
 Breakfast
Breakfast
 Supplements
Supplements
 Clothes on Carbs
Clothes on Carbs
 Eggs & Cholesterol
Eggs & Cholesterol
 Chocolate
Chocolate
 Food Labels
Food Labels
 Veggie Starters
Veggie Starters
 Move After Eating
Move After Eating
 Why Glucose Matters
Why Glucose Matters
 Glucose Revolution Book
Glucose Revolution Book
 The Glucose Goddess Method Book
The Glucose Goddess Method Book